Osteochondrosis is a disease with a wide spread, by the age of 35-40 it occurs to varying degrees in most people. The most likely localization of osteochondrosis is the lower cervical, upper thoracic and lower lumbar spine. The etiology of osteochondrosis, i. e. the specific causes and conditions of occurrence, is completely unknown. However, there is a direct influence of hereditary predisposition, age changes, injuries and impaired blood supply to tissues.
Changes in the central part of the intervertebral disc, namely dehydration, play a major role in the development of the disease. Remember that the disc consists of the nucleus pulposus and the annulus fibrosus surrounding it. Due to drying, the disc loses its shock-absorbing functions, which leads to gradual destruction. In the development of the disease, four stages are distinguished, which differ in certain changes in the disc and in the adjacent tissues. The severity of osteochondrosis of the spine, symptoms and treatment directly depend on the stage of development of the pathology.

Symptoms and causes of osteochondrosis of the spine
Let's briefly consider the stages of progression of osteochondrosis in terms of anatomical changes.
- First stage. The formation of cracks in the inner layers of the annulus fibrosus and in the nucleus pulposus. Penetrating into the cracks, the core irritates the nerve endings of the fibrous ring;
- Second phase. As additional irritation of the annulus fibrosus occurs due to the pathology of the nucleus pulposus, vertebral fixation deteriorates. There is abnormal mobility of the spine;
- Third stage. Gradual damage to the annulus fibrosus. There is a protrusion of the nucleus (protrusion) beyond the anatomical limits of the annulus fibrosus, and then there is a rupture of the annulus and the formation of an intervertebral hernia (extrusion);
- Fourth stage. There is a spread of degenerative changes in the surrounding tissues - vertebrae, ligaments, nerves, blood vessels. As a result of chronic inflammation, the intervertebral disc is scarred, leading to the development of fibrosis.
Depending on the location of the spine, there are 3 types of osteochondrosis:
- cervical osteochondrosis;
- thoracic osteochondrosis;
- Lumbar osteochondrosis.
It is worth noting that some sources distinguish the fourth type - sacral osteochondrosis.

Cervical osteochondrosis |
Thoracic osteochondrosis |
Lumbar osteochondrosis |
|---|---|---|
|
The main types of osteochondrosis are considered cervical and lumbar. However, the thoracic spine is under constant stress and is prone to the early development of gross degenerative changes, especially in young people. Due to the peculiarities of the development of changes in the chest, neurological symptoms appear in the late stage of the disease. In most cases, the disease occurs after an injury (for example, as a result of lifting too much weight).
|
Abnormalities are most often observed in the lumbar spine.
|

It was mentioned earlier that the etiology of osteochondrosis is not fully known. However, we can indicate the main causes of osteochondrosis of the spine, with a proven effect on the development of the disease:
- Regular dynamic and static loads on the spine of varying intensity. For example, the work of a loader (carrying loads) or a miner (taking unnatural positions for hours and a huge physical load), a driver (vibrations and a sedentary lifestyle) or an office worker (sedentary sedentary lifestyle;
- back injury;
- Weak physical development or overweight;
- Failure to observe correct posture and stooping;
- Flat feet and muscle imbalance as a result leads to an uneven distribution of the load on the different parts of the spine;
- genetic characteristics;
- Hypothermia leads to more intense symptoms of osteochondrosis;
- Finally, the human aging process.
Diagnosis of osteochondrosis of the spine
The preliminary diagnosis of the disease (osteochondrosis) is made based on the patient's complaints, his examination and palpation of the spine. Also, the affected part of the spine can be identified due to the topography of the distribution of pain, which is able to say exactly where (in the vertebrae of the neck, chest, lower back) nerve compression has occurred.
The main diagnostic method for diagnosing osteochondrosis is X-ray examination. Degenerative changes in the intervertebral joints, discs, narrowing of the intervertebral canal, sclerotic changes in the tissues of the spine are noted on the X-ray of the spine. At the same time, recognizing lesions of the spine (especially at an early stage) is always difficult, since the processes taking place in this case are characteristic of a number of other diseases (tumors, metastases, ankylosing spondylitis, tuberculous lesions).

On the frontal X-ray images, irregularities of the plates, increase or sharpening of the spinal processes are detected. In profile images, height reduction, change in shape, disc herniation, osteophytes, and other changes in the vertebral body are noted. Small degenerative changes are not visible on an ordinary X-ray, and an X-ray with contrast is used to detect them. The most complete information can be given by discography - an X-ray examination with the introduction of a contrast substance through a puncture directly into the intervertebral disc.
Another examination of the spine is a functional x-ray method. Thanks to the X-ray taken with maximum flexion and extension of the spine, it is possible to determine the mobility or immobility of the intervertebral space.
The most modern and high-tech research methods are computed tomography (hereinafter referred to as CT) and nuclear magnetic resonance (hereinafter referred to as MRI). Although the first machines for computed tomography and nuclear magnetic resonance appeared in the 1970s and 1980s, the technologies are still actively developing and improving, while remaining quite inaccessible to the general population due to the high cost of research or the lack of machinesin local hospitals.
Methods of treatment of osteochondrosis of the spine
The treatment of osteochondrosis is a long periodic complex process. It is aimed at reducing and eliminating the consequences of changes in the intervertebral disc. Namely inflammation, tightness, poor blood flow, muscle spasms. Many types of therapy can help in this process, including the methods of Oriental healers. In the treatment of osteochondrosis, the patient needs complete rest.
For the most part, the treatment is carried out with non-invasive methods, such as drug therapy, antiparasitic therapy, physical therapy, etc. Invasive therapy, that is, surgical operations, is rarely resorted to. For example, in such cases when the intervertebral hernia lasts more than six months and conservative treatment does not give a positive effect.
Osteochondrosis of the spine and its treatment are performed by doctors with various specialties: neurologist, orthopedist, vertebrologist, chiropractor, etc. However, the diagnosis, the appointment of tests and examinations is usually carried out by a neurologist, as well as by a vertebrologist, if there is a doctor with such a specialty in the clinic, due to his specialization in diseases of the spine.
Summarizing, we can say that the treatment of osteochondrosis is divided into the following main categories:
- Reduction of pain syndrome;
- Eliminate spasms;
- Eliminate inflammation;
- Reduction of squeezing;
- Improved blood flow;
- Prevent further deterioration.
Let's look at commonly used treatments, each covering one or more of the items on this list.
Physiotherapy treatment
Physiotherapy procedures are aimed at improving blood microcirculation in the area of the affected spine, eliminating pain and relieving swelling. Physiotherapy also helps to reduce the doses of the drugs used. There are dozens of types of physical therapy. Here are some of them:
- Reflexology is an impact on acupuncture points with needles, electricity, laser. Helps relieve spasm and improve blood flow;
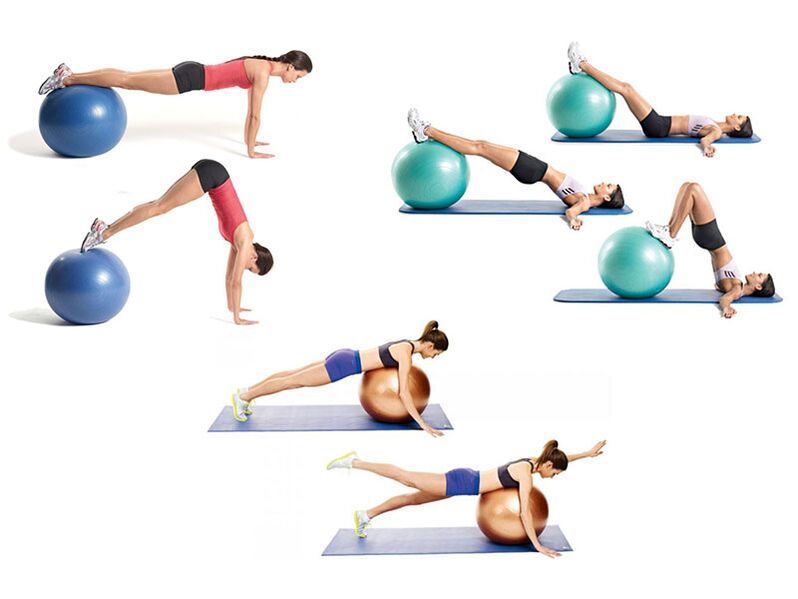
- Kinesitherapy is treatment through movement and special physical exercises. In fact, this is therapeutic gymnastics, but in an expanded sense. This includes training on simulators, exercises in groups under the guidance of a doctor, stretching the spine;
- Therapeutic swimming. It allows you to perform exercises with a spinal cord injury for those patients who find it difficult to do them. For example, the elderly, overweight or disabled people. It is important to note that due to the lifting force of the water there is an even distribution of the load on the spine;
- Impulse current therapy, UHF therapy, neurostimulation, magnetotherapy, massage, etc.
Acupuncture
A unique method that came from Eastern medicine. Its essence consists in the use of special very thin needles that enter special points of the body, literally under the influence of gravity. These points were discovered by the millennial experience of Eastern healers, later proven by official medicine. Acupuncture helps to eliminate even unbearable pain, has a positive effect on the nervous system as a whole and nervous diseases.
Surgical intervention
Surgery is indicated only in the absence of a positive effect of non-invasive treatment or in severe complications. The main method of surgical treatment is discectomy - removal of a damaged disc. However, even after surgery with minimally invasive methods, rehabilitation will take at least 6 months.
At the same time, the operation will not eliminate the need for regular treatment of osteochondrosis. Because before the operation there is always a clear task to remove a specific defect: hernia, deformation, subluxation, etc. The operation does not affect the general process of degeneration of the cartilage tissue of the spine.
Medical treatment
This type of treatment is most effective in the short term. Medicines immediately reduce pain, remove inflammation, relieve spasms, etc. However, as soon as they are canceled, in the absence of other procedures necessary for the treatment of osteochondrosis, their effect will quickly disappear. At the same time, you cannot spend your whole life on drugs, sooner or later they will have side effects on the body.

Medications can be classified as both primary and secondary treatments. They are often necessary to improve the patient's life. They are used to relieve pain (therapeutic blockade), eliminate inflammation, relieve muscle spasms, improve blood flow. In recent years, another type of medicine - chondroprotectors - has been increasingly used. However, a long-lasting permanent effect cannot be achieved with medication alone.
Treatment at home
Home treatment of osteochondrosis consists of manual therapy (exercise therapy, Schantz collar), acupuncture and vacuum therapy. These methods help to improve blood circulation and reduce congestion in the muscles and spine. As a result, tissue regeneration is significantly improved.
The listed procedures in combination with drugs provide effective treatment that relieves unpleasant symptoms and improves the general condition. In this case, special attention should be paid to proper nutrition and regulation of excess weight.
Physiotherapy
Thanks to gymnastics, the mobility of the vertebrae is restored, the muscles and their circulatory system are strengthened. The latter is of great importance, because the spinal column is deprived of the blood supply system and the intervertebral disc can receive nutrients only through the adjacent tissues. In this case, it is necessary to distinguish between therapeutic exercises and any other training.

Manual therapy
One of the most effective methods. Because the manual therapist affects the muscles, ligaments and bones. Improves posture, restores the "normal" structure of the skeleton, relieves excess muscle tension. Including, it directly affects the vertebrae.
Manual therapy of osteochondrosis should be carried out regularly, from once a year to several, depending on the need. It should be noted that this is not a one-time procedure, multidimensional, lasting 10-20 sessions. Only then will there be a positive long-term effect.

























